Shoulder Sonography: Why We Do It
Sharlene A.
Teefey, MDMallinckrodt Institute of Radiology,
J Ultrasound Med 2012; 31:1325–1331
One of
the most common causes of shoulder pain is rotator cuff disease. It is the
third most prevalent musculoskeletal disorder after low back and neck pain.
Shoulder pain is usually due to one of several causes: subacromial impingement
and bursopathy, tendinopathy, a tendon tear, a frozen shoulder, ligamentous
instability, and osteoarthritis. Rotator cuff disease (tendinopathy or tear)
highly correlates with increasing age.
In one study, the average age for patients with a painful unilateral partial-
or full-thickness tear was 58.7 years, and it was 68.7 years for those with
bilateral partial- or full-thickness tears.
This study also showed that patients with a painful unilateral full-thickness
tear had a 35.5% prevalence of an asymptomatic tear on the contralateral side.
This is important because a substantial number of patients with asymptomatic
tears become symptomatic after short-term follow-up (which has been associated
with tear size progression) and have deterioration of shoulder function.
There
are several imaging techniques that can be used to diagnose rotator cuff
disease, including sonography, magnetic resonance imaging (MRI), magnetic
resonance arthrography, and computed tomographic arthrography. This article
will focus on the role of sonography in evaluating the patient with shoulder
pain, in particular, rotator cuff disease.
Accuracy of Sonography
Sonography
has become an accepted imaging technique for evaluating the patient with
suspected cuff disease. It can be used to accurately diagnose and quantify
full- and partial-thickness tears and recurrent tears in the postoperative
shoulder, determine the tear location, and evaluate the cuff muscles for fatty
degeneration. It can also be used to diagnose other cuff disorders such as
tendinopathy and calcific tendinitis and noncuff pathology of the biceps
tendon, acromioclavicular joint, posterior labrum (paralabral cyst), and
sub-deltoid bursa.
Several
studies have reported high sensitivity, specificity, and accuracy for
diagnosing full- and partial-thickness tears. A meta-analysis by de Jesus et al
showed that sonography and MRI were comparable in both sensitivity and
specificity for diagnosing full-and partial-thickness cuff tears. It is
important to accurately diagnose and characterize cuff tears for treatment
planning. Sonographic findings help the orthopedic surgeon decide whether
treatment should be surgical or nonsurgical; if arthroscopy is indicated,
sono-graphic findings help the orthopedic surgeon counsel patients regarding
surgical and functional outcomes. If a nonsurgical approach is chosen,
sonography can be used to follow patients for tear size progression. It can
also be used to evaluate the cuff muscles for fatty degeneration, which is an
important prognostic factor regarding the patient outcome; fatty degeneration
portends a poor functional outcome and places the patient at risk of a retear.
Two studies have shown that there is a good correlation between sonography and
MRI for assessing cuff muscle atrophy and fatty degeneration,
and that the diagnostic performance between the two studies was comparable for
diagnosing fatty degeneration.
Sonography
has also been shown to be very sensitive for diagnosing calcific tendinitis and
may be used to guide aspiration of calcific deposits. Aspiration has been shown
to provide prompt and long-term pain relief at 1 year. Little has been published regarding cuff tendinopathy, although it has been
described in a few textbooks. A cadaveric study comparing sonographic findings
to histopathologic changes showed a significant relationship between cuff
tendinopathy and thickening in 21 cadaver shoulders (N. Dahiga, MD, S. Teefey,
MD, W. Middleton, MD, M. Kim, MD, and C. Hildebolt, PhD, unpublished data,
2007). The diagnosis should be considered when the cuff measures greater than
5.5 mm, based on data from a study that measured cuff thickness in 100
asymptomatic men and showed a mean thickness ± SD of 4.6 ± 0.9 mm. These authors also showed that there were no significant relationships between
sex, age, and cuff thickness in the absence or presence of shoulder pain. Thus,
this value can be generalized to men and women regardless of age and the
presence of shoulder pain.
Sonography
is very accurate for diagnosing biceps tendon subluxation, dislocation, and
rupture, although it was not able to distinguish a high-grade (≥70%)
partial-thickness tear from a rupture.
It has low sensitivity for diagnosing tenosynovitis, tendinopathy, and
low-grade partial-thickness tears.
Changes
to the acromioclavicular joint such as synovitis, effusion, osteoarthritis, and
osteolysis are easily diagnosed with sonography.
A paralabral cyst, which is usually located in the spinoglenoid notch, can be
identified with sonography and aspirated under sonographic guidance for pain
relief before definitive surgery. Subdeltoid bursal disorders such as an
effusion and bursitis can readily be diagnosed with sonography.
Sonographic Technique
Shoulder
sonography is performed using a high-frequency linear array transducer. At our
institution, the patient is seated on a rotatable stool.
The radiologist stands behind the patient to scan; however, at other
institutions, the radiologist sits and faces the patient. The biceps tendon is
the first structure to be examined; the arm is slightly externally rotated with
the forearm in a supinated position resting on the thigh. This positioning
ensures optimal visualization of the bicipital groove. The tendon is initially
examined in a transverse plane from the level where it emerges beneath the
acromion to the musculotendinous junction. The transducer is gently rocked to
maintain the normal echogenicity of the biceps tendon. The transducer is then
rotated 90° to examine the tendon in a longitudinal plane. It is important to orient
the ultrasound beam perpendicular to the long axis of the tendon to visualize
the normal echogenic, fibrillar pattern. This process may require gently
pushing the inferior aspect of the transducer against the patient’s arm to
ensure that the tendon fibers are oriented perpendicular to the ultrasound
beam.
The
subscapularis tendon is imaged next. The patient’s arm may need to be further
externally rotated to optimally visualize the tendon. The transducer is
initially placed in a transverse orientation at the level of the lesser
tuberosity and moved medially along the long axis of the tendon. Internal and
external rotation of the arm confirms that the tendon is intact. The transducer
is then turned 90° to view the tendon fibers perpendicular to their long axis.
This view is useful to diagnose superior partial- or full-thickness tears.
To
visualize the supraspinatus and infraspinatus tendons, the patient is asked to
extend his or her arm posteriorly and place the palmar side of the hand on the
superior aspect of the iliac wing with the elbow flexed and directed toward the
midline of the back. When scanning the cuff tendons in their long axis, it is
important to remember that the long axis of the tendons is approximately 45°
between the sagittal and coronal planes. It is also important to recognize that
the cuff begins within a few millimeters posterior to the intra-articular
portion of the biceps tendon. This portion of the biceps tendon should be
identified when scanning in the long axis to ensure that the anterior aspect of
the cuff is visualized. The cuff should be evaluated from the most lateral
aspect of the greater tuberosity where it inserts to as far medially as
possible to ensure that more medial mid substance tears are not missed. Because
the cuff assumes a convex curvilinear course as it passes over the humeral
head, the transducer should be gently rocked to visualize the various portions
of the cuff in a plane perpendicular to the ultrasound beam as it is moved
anterior to posterior. It is also important to compress the transducer against
the deltoid muscle to detect any nonretracted tears. The transducer is then
turned 90° to visualize the cuff in a transverse (short-axis) orientation. This
view is useful to measure the width and determine the location of a cuff tear.
Next, the posterior glenohumeral joint and the posterior aspect of the
infraspinatus and teres minor tendons are evaluated from a posterior approach
with the patient resting his or her forearm on the thigh. To identify the
glenohumeral joint and the more posterior aspect of the infraspinatus tendon,
the transducer is placed immediately below the scapular spine and angled
slightly inferiorly. Internal and external rotation of the arm helps better
visualize the infraspinatus attachment and the posterior cartilaginous labrum.
Finally,
each of the posterior cuff muscles should be evaluated in long and short axes
for fatty degeneration. The transducer is first placed superior to the scapular
spine to image the supraspinatus muscle and then moved inferior to the scapular
spine to visualize the infraspinatus muscle. The transducer is then moved
slightly more inferiorly to visualize the teres minor muscle and its short
tendon, most of which attaches to the surgical neck of the humerus.
To visualize the entire tendon and its muscle, the transducer should be placed
at the level of the surgical neck in a sagittal orientation and moved lateral
to medial along the muscle.
The
acromioclavicular joint can be imaged in both coronal and sagittal planes but
is best evaluated when the transducer is oriented along the long axis of the
clavicle. This view optimizes visualization of the joint space, synovium,
capsule, and bony margins of the joint.
Figure 2: Full-thickness cuff tear in a
69-year-old woman. A, The longitudinal image
shows the cuff tear (between cursors). The torn tendon end is not surrounded by
fluid. B, The transverse image shows
the width of the tear (between cursors).
Sonographic Findings of Shoulder
Disorders
Most
cuff tears begin approximately 15 mm posterior to the intra-articular portion
of the biceps tendon.
There may be associated bony changes on the greater tuberosity. On sonography,
a full-thickness cuff tear is characterized by a focal defect created by a
variable degree of retraction between the torn tendon ends. When there is fluid
between the torn tendon ends, it is easy to visualize a tear (Figure 1).
In the absence of an effusion, the deltoid muscle and peribursal fat occupy the
space created by the defect and oppose the overlying humeral head cartilage (Figure 2).
If the subdeltoid synovial tissue is thickened and inflamed, the tissue will
abut the cartilage, and on sonography, a subtle loss of the normal convexity of
the cuff or flattening of the cuff will be visualized. Nonretracted tears are
difficult to identify. It is important to compress the deltoid with the
transducer in an attempt to show the defect. Less often, a tear will occur more
medially within the mid substance of the cuff; thus, it is important to
evaluate the cuff where it exits beneath the acromion to the lateral aspect of
the greater tuberosity. In a patient with a massive tear, the cuff is often not
visualized and is retracted beneath the acromion on longitudinal views (Figure 3).
Because of the size of the tear, it is usually not possible to measure an
accurate width. These cuff tears are often chronic and most commonly seen in
elderly patients. Subscapularis tears are uncommon and usually occur in patients with massive
cuff tears or recurrent anterior shoulder dislocation. It is important to
diagnose a subscapularis tear because it may alter the surgical approach.
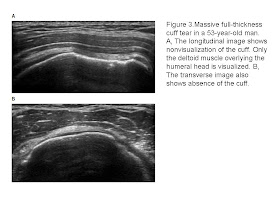
Figure 3: Massive full-thickness cuff
tear in a 53-year-old man. A, The longitudinal image
shows nonvisualization of the cuff. Only the deltoid muscle overlying the
humeral head is visualized. B, The transverse image also
shows absence of the cuff.
Partial-thickness
tears can be more difficult to identify than full-thickness tears. These tears
usually occur along the deep side of the cuff at the level of anatomic humeral
neck and can be recognized as distinct hypoechoic or mixed hyperechoic and
hypoechoic defects on both longitudinal and transverse views (Figure 4).
It is important not to mistake anisotropy for a partial-thickness tear;
anisotropy produces a much less well-defined, uniformly hypoechoic region in
the deep portion of the cuff. By angling the transducer such that those fibers
become perpendicular to the ultrasound beam, normal tendon fibers will be noted
inserting onto the greater tuberosity. A partial-thickness tear that involves more
than 50% of the substance of the cuff may be compressible with the transducer
and simulate a full-thickness tear. Misdiagnosing an extensive
partial-thickness tear for a full-thickness tear is usually not clinically
relevant because it is often treated as if it were a full-thickness tear.
Partial-thickness tears may occur on the bursal side of the cuff but are much
less common; small bursal-side tears are often difficult to distinguish from
small full-thickness tears because both produce a focal defect or concavity on
the bursal side of the cuff. Linear tears may also occur within the substance
of the cuff but are more difficult to visualize than on MRI.
Figure 4: Partial-thickness
articular-side cuff tear in a 55-year-old woman. A, The longitudinal image shows a distinct
hypoechoic defect in the cuff (between cursors). B, The transverse image shows the width of the tear
(between cursors).
Fatty
degeneration of the cuff muscles can be diagnosed as described by Strobel et
al.These authors evaluated the visibility of the muscle contours, pennate pattern,
and central tendon and assessed the echogenicity of the cuff muscles in
comparison to the deltoid muscle to grade the degree of fatty degeneration.
When fatty degeneration is severe, one or more muscles will become
homogeneously hyperechoic (Figure 5).
A recent study showed that fatty degeneration of the cuff muscles is closely
associated with the tear size and location. The greater the size of the tear, the greater the risk of fatty degeneration,
and the closer the tear begins to the intra-articular portion of the biceps
tendon, the greater the risk of fatty degeneration. The mechanism for the
latter may be due to disruption of the rotator cable insertion (the anterior
part of the supraspinatus tendon is the site of the anterior cable insertion),
resulting in greater retraction of the tendon and subsequent fatty degeneration
over time.
Although
little has been published on the sonographic appearance of tendinopathy, on the
basis of our observations, it may be a focal or diffuse process; the cuff is
typically thickened, heterogeneous, and hypoechoic (Figure 6).
Calcific tendinitis may be diagnosed when echogenic foci of varying size that
may or may not shadow are visualized within the substance of the tendon. The
calcifications are often located at the most lateral aspect of the greater
tuberosity.
Figure 5: Marked fatty degeneration of
the supraspinatus tendon in a 70-year-old man with a full-thickness cuff tear.
The longitudinal image shows a homogeneously echogenic supraspinatus muscle.
Disorders
of the biceps tendon are commonly associated with rotator cuff disease and are
important sources of shoulder pain. When the biceps tendon is thickened and
hypoechoic, tendinopathy should be considered. Tendinopathy usually occurs in
patients with large chronic cuff tears. Intrasubstance tears may also occur and
appear as linear hypoechoic defects. Tenosynovitis is often associated with an
effusion. A thickened tendon sheath with or without flow on color or power
Doppler imaging is diagnostic of tenosynovitis (Figure 7).
Tendon subluxation is considered present when the tendon partially extends
above a line drawn from the lesser to the greater tuberosity and dislocated
when perched or medial to the lesser tuberosity. Tendon rupture can be
diagnosed when the bicipital groove is empty; however, a 70% or greater
high-grade partial-thickness tear cannot be distinguished from rupture because
the few remaining fibers are usually not visible on sonography.
Figure 6: Marked tendinopathy in a
75-year-old man. The longitudinal image shows a hypoechoic and very thickened
cuff.
The
subdeltoid bursa is a potential space and normally does not contain fluid. The
presence of fluid is abnormal, and if there is concern for infection,
sonography can be used to provide guidance for aspiration. Bursitis can be an
overlooked cause of shoulder pain. It can be diagnosed if the subdeltoid bursa
is thicker than the humeral head cartilage (Figure 8).
Shoulder abduction with real-time observation helps distinguish the cuff from
thickened bursa.
Figure 7: Tenosynovitis of the biceps
tendon sheath in an 81-year-old woman. The transverse image shows thickening of
the biceps tendon sheath. There is increased flow of the thickened synovium on
color Doppler imaging.
A
paralabral cyst is caused by a posterior capsulolabral avulsion or tear with
subsequent leakage of fluid. It is best seen from a posterior approach; the
transducer should be placed at the level of the infraspinatus muscle. These
anechoic cysts typically occur in the spinoglenoid notch and may extend into
the supraspinous or infraspinous fossa. It is important to evaluate the
supraspinatus and infraspinatus muscles for fatty degeneration, which may occur
if the suprascapular nerve (a mixed motor/sensory nerve) is compressed by the
cyst.
The
acromioclavicular joint may become infected or inflamed, causing the joint to
distend with fluid and the capsule to bulge. The fluid is easily aspirated under sonographic guidance. A synovial cyst,
which may be anechoic or contain debris on sonography, if found to communicate
with the acromioclavicular joint, should prompt investigation of the rotator
cuff because it is associated with a longstanding full-thickness cuff tear.
Osteolysis appears as joint space widening and irregularity and erosions of the
bony margins.
Figure 8: Bursitis in a 34-year-old
woman. The transverse image shows marked thickening of the subdeltoid bursa
(between cursors).
Conclusions
In
summary, sonography is an excellent modality for diagnosing rotator cuff
disease. It is preferred by patients,
accurate, noninvasive, rapidly performed, and less expensive than MRI.
Furthermore, it is a dynamic, global examination and can provide bilateral
information. There is also the opportunity to interact with the patient and
explain the results of the examination. However, it is important to recognize
that the learning curve is long and steep, and results are operator dependent.
It is also more difficult to visualize the entire cuff in obese patients and in
patients with decreased range of motion, and evaluation of the labrum, joint
capsule, ligaments, bone, and cartilage is limited. Thus, whereas sonography
and MRI have comparable accuracy for diagnosing rotator cuff disease, these
tests should be viewed as complementary rather than competitive. Which test to
perform should be based on the clinical information sought and the inherent
strengths and weaknesses of each test.







Không có nhận xét nào:
Đăng nhận xét