Discussion
Our study is unique in that it is a surveillance study of 125 consecutive patients whose evaluation entailed a global assessment encompassing clinical and ultrasound examination. Unlike previous works,2–6 it was performed to evaluate a protocol for head-to-toe ultrasound examination performed by a team of ICU physicians experienced in ultrasonography. Real-time ultrasound evaluation (within 12 h of admission) was done by the attending physician. The approach is based on the assumption that intensive care physicians with enough expertise can interpret sonographic images.
Ultrasound training is not mandatory for ICU physicians in Italy, although proposals for graded competence have been advanced. Since 2000, the Society for Academic Emergency Medicine guidelines for physician training in emergency ultrasonography12 have informed the continuing medical education program of our ICU physicians. During their time in the course, physicians are required to perform 150 practice sections, including 60 heart, 10 chest, 60 abdomen, and 20 peripheral vein ultrasound examinations. After the course, the physicians receive 1 yr of tutored instruction.
Drawn up in 2008, the ICU-sound protocol was tested for 6 months before entering daily clinical practice. Our data suggest that the protocol is not excessively time-consuming: a mean duration of 19.5 min to complete the scan is acceptable considering the protocol's complexity. Patient- and environment-related ultrasonography limitations had little influence on the majority of the ultrasound examinations in this study.
We used optic nerve sonography as an additional noninvasive diagnostic tool to detect increased intracranial pressure preceding emergency computed tomography or the decision to start invasive monitoring of intracranial pressure. Ultrasound examination revealed new findings of optic nerve sheath enlargement in six cases, in all of which computed tomography showed unknown intracranial hypertension, demonstrating the importance of this easy-to-perform ultrasound evaluation at admittance to a general ICU.
Image Tools
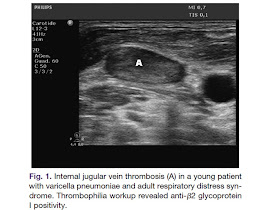
Two cases of unknown deep venous thrombosis were identified, one an internal jugular vein thrombosis (fig. 1). Upper extremity venous thrombosis is thought to be quite rare, but a recent report found that 18% of all cases involve upper extremity thrombi. Patients in the ICU setting are especially vulnerable to developing upper extremity thrombosis, and the clinical symptoms associated with an upper-extremity clot are frequently absent because of the extensive collateral network. A combined strategy using echocardiography and venous ultrasonography is a reliable method for diagnosing pulmonary embolism at the bedside.
Pleural effusion is often encountered in ICU patients; the diagnosis relies mostly on an anteroposterior chest radiograph obtained at the bedside. Pleural ultrasonography, an alternative imaging modality, has been validated against chest computed tomography, the accepted reference for diagnostic methods to identify pleural disease. The prevalence of significant pleural effusions in a medical ICU varies widely from 8.4 to 62%.
In our study, effusions (small effusions less than 200 ml were not considered) were found in 35/125 patients (28%), 20 (57.1%) of whom underwent drainage and thoracenthesis. The estimated drainage volume was obtained using the formula proposed by Balik et al. It has been recently shown, however, that this formula can underestimate the volume, whereas a multiplane approach can increase the accuracy of quantifying small and moderate pleural effusion. Although more time-consuming (10 min), an accurate evaluation of effusion volume is a critical element in deciding whether to perform thoracenthesis. And it becomes even more relevant when weaning is considered, because drainage may reduce the work of breathing and increase respiratory muscle efficiency.
The decision to drain was based on our clinical practice (reduced chest wall compliance, difficult weaning, refractory hypodynamic circulatory states) or when ultrasound suggested an infectious effusion (homogeneous echogenicity, septation, fibrin strands, nodular pleural changes). Pleural effusion can cause dissociation between effective preload and cardiac filling pressures. Drainage may be effective in patients with refractory hypodynamic circulatory states, particularly when there is evidence for diastolic chamber collapse.
Image Tools
Ultrasound examination was effective in evidencing the presence of anterior pneumothorax not detected by supine anteroposterior chest radiography (three cases). This finding holds clinical relevance, because during positive pressure ventilation a small pneumothorax may progress and cause hemodynamic instability. Ultrasound has proved to be more sensitive than anteroposterior chest radiography in the diagnosis of pneumothorax and can decrease the need for computed tomography for the diagnosis of occult pneumothorax. Lower lobe parenchymal consolidation without air bronchogram visualization can be difficult to distinguish from pleural effusion on an anteroposterior chest radiograph. Ultrasonography showing consolidation (with or without pleural effusion) can help in avoiding a possible mistake because of a misread chest radiograph (fig. 2).
Image Tools
Lung sonography is a useful aid in differentiating cardiogenic respiratory failure from acute airflow limitation, consolidation, pleural effusion, or pulmonary embolism. In our study, the diagnostic efficacy of lung ultrasound to differentiate dyspneic patients is well represented. Lung ultrasound pointed out 55 new findings, enabling us to differentiate the etiologic diagnosis in patients with a generic admitting diagnosis of acute respiratory insufficiency. Combining the data from lung sonography and echocardiography can enhance the diagnostic accuracy in differentiating respiratory insufficiency (fig. 3).
Image Tools
In a previous study, transthoracic echocardiography performed by intensivists provided new information and changed management in 37% of critical patients and added useful information to an additional 47% of patients, but did not alter immediate treatment. In our study, echocardiography revealed 53 new findings, leading to changes in therapy in 11/125 patients. These data confirm the importance of transthoracic echocardiography in ICU patients.
Abdominal examination evidenced 20 new pathologic findings and induced changes in therapy in 3/125 cases. The presence of the classic signs of acute acalculous cholecystitis at ultrasound examination, together with clinical data, enabled us to identify the origin of sepsis of unknown etiology (fig. 4).
In our study, new ultrasound abnormalities were most often detected in patients with septic shock, followed by those with acute cardiac decompensation. This is not surprising, as these patients have multiple organ failure. ICU mortality was higher, but not statistically significant, in patients with two or more pathologic findings compared with patients without any findings. Mortality generally depends on the specific type of the most life-threatening abnormality, along with many other factors unrelated to ultrasound findings. Of note is that patients with no ultrasonographic pathologic findings had a better prognosis.
We plan to extend the ICU-sound protocol to include other diagnostic tools: transcranial Doppler and positive end-expiratory pressure-induced lung recruitment. Recent reports have shown, in fact, that lung reaeration can be assessed by ultrasound. It is rapid and repeatable at the bedside, does not require sedation and paralysis, and can be used to analyze dependent and not-dependent lung regions. Patients with acute lung injury, the adult respiratory distress syndrome, and pulmonary edema may benefit from ultrasound monitoring of positive end-expiratory pressure-induced reaeration; however, a limitation is that lung hyperinflation cannot be assessed.
Study Limitations
There is a potential for bias, as the operators in this study were not blinded to the patient's clinical picture, which is difficult to entirely eliminate in any use of ultrasound. The study relied only on transthoracic echocardiography; therefore, the true prevalence of cardiac ultrasound abnormalities may have been underestimated. Also, the prevalence of pleural effusion may have been underestimated with the use of a formula, which has been shown inadequate to quantify small and moderate effusions. An evaluation of the usefulness of a head-to-toe versus a focused examination was beyond the scope of this study.
The major finding of this study is the discovery of a high prevalence of unsuspected clinical abnormalities in ICU patients. Ultrasound examination permitted us to modify the diagnosis and to improve the treatment, with prompt changes in therapeutic strategy. Patient- and environment-related sonography limitations had little influence on the majority of the examinations. The test can be performed by the attending ICU physician, with minimal risk of overuse or misinterpretation. Moreover, ultrasound use in the ICU could be optimized by making ultrasonography a routine part of intensive care training during residency. In experienced hands, rapid global assessment of critical patients at ICU admittance under this ultrasound protocol holds potential for improving healthcare quality.





Không có nhận xét nào:
Đăng nhận xét