Esophageal cancer is an important cause of cancer death, with an incidence of about 8-10/100 000 and 13
300 deaths in the United States
Distant metastases, especially liver metastasis, can be diagnosed
by CT scan or MRI with high sensitivity and specificity[6]. Sensitivities of
these diagnostic means range between 74% and 85%[9]. In these series, almost
all false-negative results occurred when lesions were less than 1.5 cm in
diameter. Therefore, non-invasive detection of small metastases can be
diffi cult or even impossible. When
suspicious lesions are found by CT scan, further differentiation is possible by
additional MRI imaging [5]. Differential diagnosis of liver metastases includes
benign liver lesions, including hemangiomas, adenomas, von Meyenburg complexes
or infectious lesions e.g. miliary tuberculosis [5].
Bile duct hamartomas (von Meyenburg complexes) of the liver
are usually detected during laparotomy or autopsy as an incidental finding. Multilocular occurrence is possible although
they are rarely spread throughout the whole liver, as it was observed in our
first patient. They may be found in
normal liver tissue, but also in association with Caroli’s syndrome, congenital hepatic fibrosis (CHF) or autosomal dominant polycystic
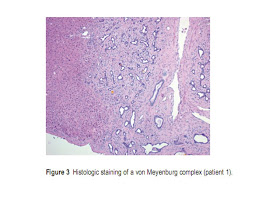
kindney disease (ADPKD) [10]. Histology of von Meyenburg complexes consists of
a variable number of dilated small bile ducts, embedded in a fibrous, sometimes
hyalinizing stroma (Figure 3).
If detected by CT scan or MRI, von Meyenburg complexes
appear as small intrahepatic cystoid lesions. The lesions are frequently located
adjacent to the portal veins, although the lesions can also be located
everywhere else [5]. However, it remains difficult to differentiate between metastases
and benign liver lesions. Moreover, small liver lesions with a diameter of less
than 1.5 cm are often not detected by CT or MRI [9].
Since the treatment of metastatic disease is completely different
from resectable esophageal cancer, liver
lesions need to be identified and characterized as early as possible.
In our presented patients, the preoperative staging did not reveal
any liver metastases. This underlines the importance of exact diagnostic
measures in cases of unexpected intraoperative findings. Besides intraoperative
ultrasound of the liver, frozen section is the gold standard for further differentiation of liver lesions of unknown origin.
Von Meyenburg complexes are defined as innocuous lesions. However,
there are about 10 reported cases of neoplastic transformation of von Meyenburg
complexes resulting in cholangiocarcinomas [2,3].
In conclusion, von Meyenburg complexes are an important
differential diagnosis of hepatic metastases. As the existence of liver
metastases is crucial for therapeutic decision making in malignant diseases, this
differential diagnosis must be carefully clarified. Since von Meyenburg complexes are usually less than 5 mm in size, they can escape
preoperative radiologic diagnostics. The macroscopic appearance of von
Meyenburg complexes can mimic liver metastasis as demonstrated in our reported
patients. This underlines the importance of intraoperative frozen sections to
make the correct diagnosis.





Không có nhận xét nào:
Đăng nhận xét