Abstract
Introduction: Ultrasonography is associated with a high
error rate in the evaluation of soft tissue masses. The purposes of this study
were to examine the nature of the diagnostic errors and to identify areas in
which reporting could be improved.
Methods: Patients who had soft tissue tumours and received ultrasonography
during a 10-year period (1999–2009) were identified from a local tumour registry.
The sonographic and pathological diagnoses were categorised as either ‘benign’
or ‘non-benign’. The accuracy of ultrasonography was assessed by correlating
the sonographic with the pathological diagnostic categories.
Recommendations from radiologists, where offered, were
assessed for their appropriateness in the context of the pathological diagnosis.
Results: One hundred seventy-five patients received
ultrasonography, of which 60 had ‘non-benign’ lesions and 115 had ‘benign’
lesions. Ultrasonography correctly diagnosed 35 and incorrectly diagnosed
seven of the 60 ‘non-benign’ cases, and did not suggest a diagnosis in 18
cases. Most of the diagnostic errors related to misdiagnosing soft tissue
tumours as haematomas (four out of seven). Recommendations for further
management were offered by the radiologists in 144 cases, of which 52 had ‘non-benign’
pathology.There were eight ‘non-benign’ cases where no recommendation
was offered, and the sonographic diagnosis was either incorrect or
unavailable.
Conclusions: Ultrasonography lacks accuracy in the
evaluation of soft tissue masses. Ongoing education is required to improve awareness
of the limitations with its use. These limitations should be highlighted
to the referrers, especially those who do not have specific training in this
area.
Key words: diagnostic error; haematoma; neoplasm, connective
and soft tissue; ultrasonography.
DISCUSSION
Ultrasonography lacks accuracy in the evaluation of soft tissue masses
due to the non-specific nature of many imaging findings. The present study has
reaffirmed our previous observations that ultrasonography has a high error rate
in distinguishing non-benign from benign lesions. Despite our earlier
experiences and the increased awareness of the limitations of ultrasonography,
no significant improvement in error rates was observed between the current and
the previous study periods.
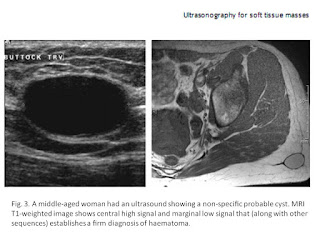
A common diagnostic error involves mistaking solid tumours for
haematomas, sometimes resulting in diagnostic delay and suboptimal management.
In a review of 31 cases of soft tissue tumours masquerading as haematoma, Ward et al. found that misdiagnosis was associated with diagnostic delays
averaging 6.7 months; furthermore,
neither ultrasonography nor magnetic resonance could reliably differentiate
soft tissue tumours and haematoma.[3] It may be useful to correlate
with clinical history such as recent trauma and examination findings such as
subcutaneous ecchymosis.[4] However, it is important to note
that a history of trauma may be incidental, and ecchymosis can also occur with
tumoural bleeding.[3]
Given these difficulties, it is not surprising that many radiologists
err on the side of caution when confronted with a soft tissue mass on
ultrasonography. Of the 115 patients with histologically benign lesions,
ultrasonography suggested a suspicious diagnosis or recommended further
evaluation in 92 cases (80%, positive likelihood ratio 1.1). A ‘positive’
ultrasonography result per se therefore adds little diagnostic value in the
evaluation of patients with soft tissue masses. On the other hand, one should
be cautious to assign a ‘negative’ result to a study without providing specific
guidance or recommendation. Notably, diagnostic delays have been observed in
false negative cases when such recommendation has not been explicitly made.
This is particularly relevant in our local practice, where non-specialists
(e.g. general practitioners) contribute up to 60% of the referrals for
ultrasonography examination for soft tissue masses. In these circumstances, a
short comment such as the following may help guide the referrers in appropriate
cases:
… The findings are non-specific. If the lesion does not resolve
rapidly, or if the radiological diagnosis does not fit the clinical picture, a
referral to a specialist surgeon is recommended and further imaging such as MRI
may be appropriate.
Despite its limitations, ultrasonography may serve specific roles in
the work-up of soft tissue masses. First, ultrasonography can confirm the
presence of a mass, which can sometimes be difficult to ascertain clinically.
Second, ultrasonography can differentiate cystic lesions from solid lesions.
Third, ultrasonography can often reliably diagnose lesions with certain
well-characterised sonographic features. For instance, a cyst adjacent to a
tendon may suggest a ganglion, and a superficial well-defined echogenic mass
may suggest a lipoma. It should be noted that the majority of these lesions are
satisfactorily managed in the community without being referred to the registry,
and are therefore excluded in this review. Fourth, ultrasonography may be used
to guide biopsy of the lesions. This is particularly valuable in targeted
biopsy of large, heterogeneous tumours.[5]
Ultrasonography has been utilised in tumour follow-up in the research
setting. It has been used to detect tumour recurrence[6, 7] and monitor regression of
tumour neovascularity induced by therapy for musculoskeletal sarcoma.[8] Ultrasonography may also be used
in conjunction with MRI when susceptibility artefacts from orthopaedic hardware
prevent evaluation of specific areas following surgery.[8] It has been suggested that
colour Doppler flow imaging and spectral wave analysis may allow assessment of
blood flow within soft tissue masses and, by inference, differentiate between
malignant and benign tumours.[9]
In summary, ultrasonography has specific roles in the evaluation of
soft tissue masses. However, aside from the recognisable entities of ganglion,
superficial lipoma and obvious peripheral nerve sheath tumour, ultrasonography
of soft tissue masses remains non-specific with respect to malignancy. Ongoing
education is prudent to improve our understanding of its limitations and
pitfalls. In addition, it may be important to highlight these limitations to
the referrers, especially if they have no specific training in the management
of soft tissue masses.




Không có nhận xét nào :
Đăng nhận xét