July 17, 2020 -- The findings on initial lung scans with point-of-care ultrasound (POCUS) can predict which patients with COVID-19 are at a greater risk of death, according to a prospective study from Italy published on July 15 in Ultrasound in Medicine & Biology.
Physicians in Rome performed lung ultrasound scans on 41 adult patients who visited a tertiary emergency department with symptoms of the novel coronavirus disease. Patients who later died or were later admitted to the intensive care unit (ICU) had significantly worse pathological findings on their initial scan.
"Our study shows that [lung ultrasound scan] is able to detect COVID-19 pneumonia and to predict, during the first evaluation in the emergency department, patients at risk of intensive care unit admission and death," wrote the authors, led by Nicola Bonadia, from the department of emergency medicine at Agostino Gemelli University Policlinic.
Physicians performed point-of-care ultrasound (POCUS) scans on all patients with suspected cases of COVID-19 who visited the emergency department in March. The emergency department staff used a pocket device with a wireless 6-MHz convex probe and followed a previously described lung ultrasound protocol that includes 14 chest areas.
Each scanned area received a numeric score of 0 to 3 based on the severity of the findings in that section. A higher lung ultrasound score (LUS) signified worse disease severity, with a score of 3 indicating dense or large areas of white lung with or without subpleural consolidations.
The authors analyzed the lung ultrasound findings from 41 patients with a positive SARS-CoV-2 test result and known outcomes. They specifically excluded children and patients with less than six months life expectancy due to preexisting chronic conditions, such as advanced cancer or dementia.
More than 90% of adult patients with COVID-19 had at least one area with an abnormal lung ultrasound finding. Pathological findings occurred in all 14 scanned areas but were most prominent in the lateral lung regions, the authors noted.
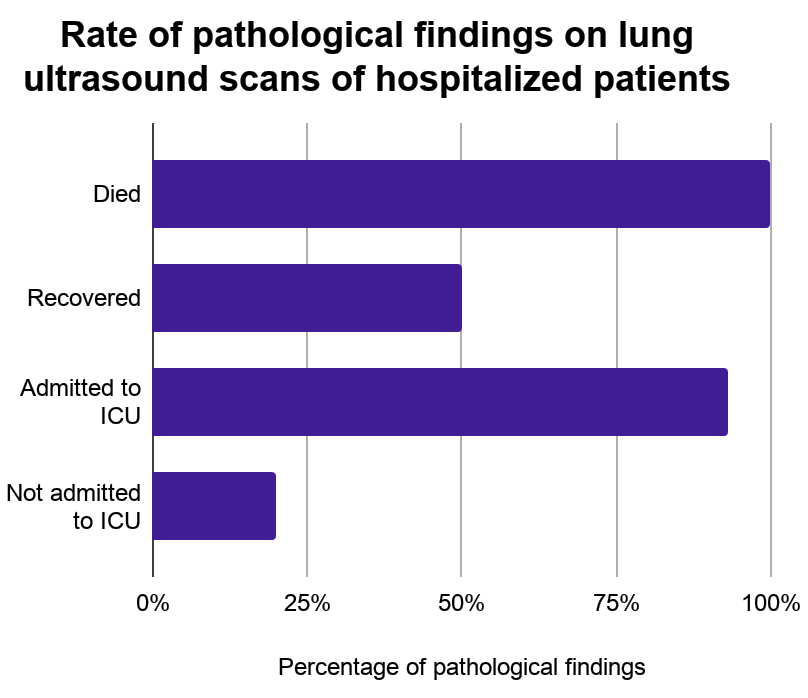
Patients with fatal cases of COVID-19 had pathological findings in 100% of scanned areas, compared with just 50% of scanned areas in discharged patients. These patients also had a mean lung ultrasound score of 1.43, compared with 1.0 in discharged cases.
Similarly, patients admitted to the ICU had pathological findings in 93% of scanned areas, compared with just 20% of areas in patients not admitted to the ICU. ICU patients also had a mean LUS of 1.36, compared with 1.0 in non-ICU patients.
Based on their findings, the authors determined the cutoff for a strict definition of COVID-19 pneumonia should be an LUS of 0.4 and a pathological findings rate of at least 20%. Furthermore, no study participants died if they had a mean LUS less than 1.1 and an average pathological rate under 70%.
The authors cautioned their study took place at one institution and had a small sample size. Nevertheless, the findings may help health professionals better triage patients with COVID-19 and spur future studies to evaluate whether lung ultrasound scores can guide patient treatment and admission decisions.
"We found a significant correlation between ultrasound findings and severity of the disease, assessed as mortality and need for ICU admission," the authors wrote. "To our knowledge, this is the first study describing the predictive role of LUS in patients with COVID-19."
Không có nhận xét nào :
Đăng nhận xét