February 15, 2022 -- Ultrasound found links between symptoms of long COVID-19 disease and the effects of the SARS-CoV-2 virus on the vagus nerve, according to research that will be presented at the European Congress of Clinical Microbiology & Infectious Diseases in April. A team led by Dr. Gemma Lladós from Germans Trias i Pujol Hospital in Badalona, Spain found that COVID-19 patients with symptoms of vagus nerve dysfunction mediated by SARS-CoV-2 also had nerve thickening, decreased esophageal and diaphragmatic mobility, and reduced maximum inspiratory pressures values.
"We need to improve our understanding of the mechanisms that may cause the persistence of symptoms to help patients and find interventions that can prevent and treat vagus nerve dysfunction," Lladós told AuntMinnie.com.
Stretching from the brain to the torso and into the heart, the vagus nerve plays an important role in bodily functions. These include controlling heart rate, speech, the gag reflex, transferring food from the mouth to the stomach, moving food through the intestines, and sweating, among others.
Post-COVID syndrome, also commonly known as long COVID, affects 10% to 15% of COVID-19 survivors, researchers wrote. Symptoms include persistent voice problems, difficulty in swallowing, dizziness, tachycardia, low blood pressure, and diarrhea.
However, the researchers said the mechanism that causes long COVID is currently unknown. Therefore, Lladós et al wanted to determine the morphological and functional activities of the vagus nerve in their pilot study of long-COVID patients with dysfunction, using ultrasound and functional tests.
They looked at data from 22 patients who were selected from a cohort of 228 individuals who had at least one symptom suggestive of vagus nerve dysfunction. Patients had a median age of 44 years and presented between March and June 2021. Out of these, 20 were women.
| Most common vagus nerve dysfunction symptoms in patients presenting with long COVID | |
| Diarrhea | 73% |
| Tachycardia | 59% |
| Dizziness | 45% |
| Difficulty swallowing | 45% |
| Persistent voice problems | 45% |
The study authors found that 19 patients had at least three dysfunction-related symptoms, and the median prior duration of symptoms was 14 months.
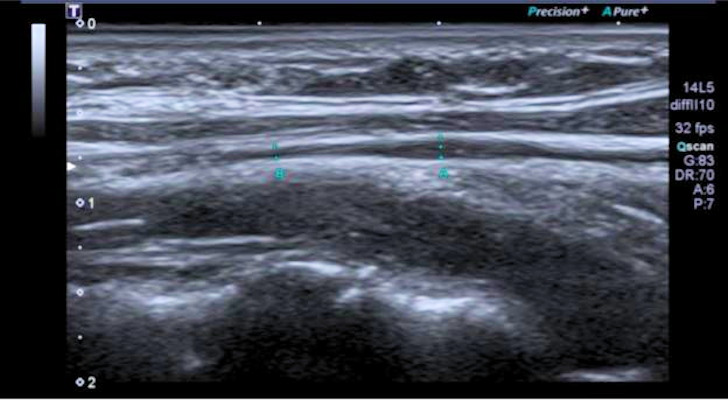
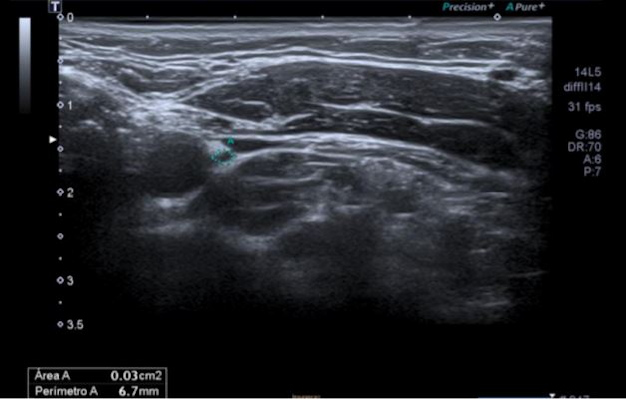
Six patients had mild vagus nerve thickening and higher echo on neck ultrasound scans. Thoracic ultrasound, meanwhile, showed flattened diaphragmatic curves in 10 patients. Ten out of 16 patients also showed reduced maximum inspiratory pressures.
"Radiologists may find by ultrasound in the lateral cervical area some images over the vagus nerve reflecting mild reactive inflammatory changes," Lladós said. "In addition, a flattened diaphragmatic curve visualized by chest ultrasound could translate into decreased diaphragmatic mobility during respiration."
The team also found eating and digestive dysfunction in patients, with 13 out of 18 having indication of trouble swallowing. Eight out of 19 patients also reported having their ability to deliver food to the stomach impaired, two of whom had difficulty swallowing. Acid reflux was also seen in nine of 19 patients, four of whom reported difficulty delivering food to the stomach and three having hiatal hernia.
The researchers also found abnormalities in voice function for eight out of 17 patients, seven of these reporting dysphonia, or persistent voice problems.
Lladós told AuntMinnie.com that the team wants to compare their results with healthy controls and with patients infected by SARS-CoV-2 without the persistence of symptoms. He said the aim is to know if there is more morphological and functional involvement of the vagus nerve in infected patients.
The team's findings will be presented at the European Congress of Clinical Microbiology & Infectious Diseases in Lisbon, Portugal, which will be held April 23-26.

Không có nhận xét nào :
Đăng nhận xét