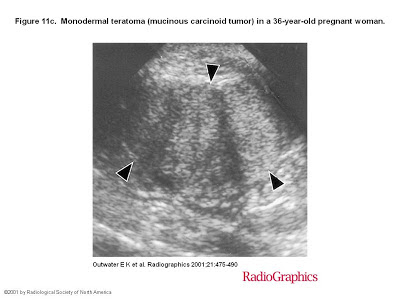
Figure
4d. Mature cystic teratoma of the right ovary in a 19-year-old
pregnant woman. (d) Photograph of the
gross specimen shows yellowish, pasty sebaceous material (black arrowhead) and
hair (white arrowheads) within the cyst cavity, findings that account for the
fat echogenicity and signal intensity seen at US and MR imaging. Two molar teeth
are also evident (arrows).
Figure 4(a) Sagittal transabdominal US
Abstract
Ovarian teratomas
include mature cystic teratomas (dermoid cysts), immature teratomas, and
monodermal teratomas (eg, struma ovarii, carcinoid tumors, neural tumors). Most
mature cystic teratomas can be diagnosed at ultrasonography (US
At computed tomography (CT), fat attenuation within a cyst is diagnostic. At magnetic resonance (MR) imaging, the sebaceous component is specifically identified with fat-saturation techniques. TheUS
At CT and MR imaging, immature teratomas characteristically have a large, irregular solid component containing coarse calcifications. Small foci of fat help identify these tumors. TheUS US
At computed tomography (CT), fat attenuation within a cyst is diagnostic. At magnetic resonance (MR) imaging, the sebaceous component is specifically identified with fat-saturation techniques. The
At CT and MR imaging, immature teratomas characteristically have a large, irregular solid component containing coarse calcifications. Small foci of fat help identify these tumors. The
Most mature cystic teratomas can be diagnosed
at US. However, the US
In a prospective US study that made use of
these criteria, Mais et al (20) found a sensitivity of 58% and a specificity of 99% in the
diagnosis of mature cystic teratoma. Numerous pitfalls have been described in
the US